Arq. Bras. Cardiol. 2020; 115(6): 1205-1207
Pulmonary Thromboembolism in a Young Patient with Asymptomatic COVID-19
Case presentation
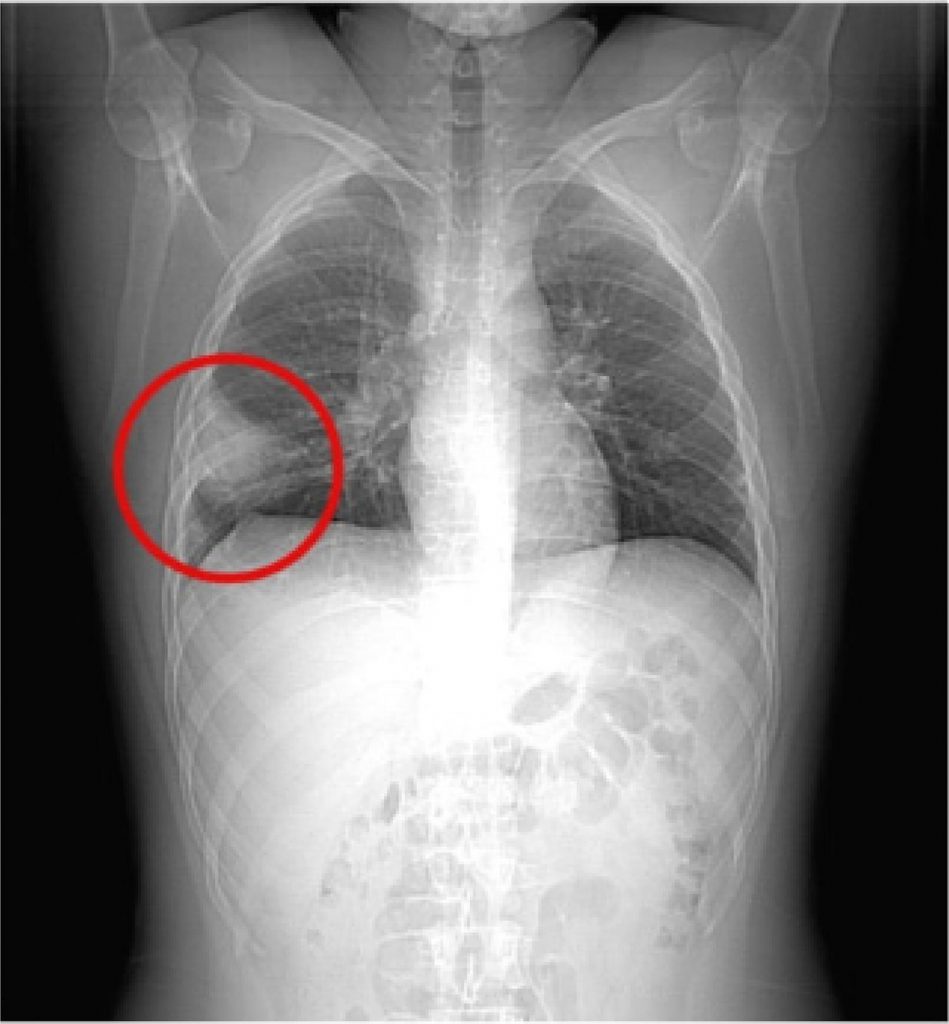
A male patient, 22 years old, with no previous comorbidities and medication use was referred to our hospital on 06/24/2020. Without symptoms, on 06/12/2020 he was diagnosed with COVID-19 after a PCR screening test required at his company and remained in bed rest during most of his isolation. He continued asymptomatic for 11 days; however, on 06/24/2020, he was admitted to the emergency department with ventilatory-dependent pain in the right hemithorax. Vital signs revealed hypertension (132/78 mmHg), tachycardia (127 bpm), hypoxia (SpO2of 90% at ambient air), and fever (38.7 °C). On physical examination, attention was drawn to the decrease in breath sounds in the right hemithorax during pulmonary auscultation. Padua and Wells risk stratification scores were applied, and the criteria indicated a low risk (3 points) and a moderated risk (6 points), respectively. D-dimer (6.652 μg/L), C-Reactive Protein (94 mg/L) and Troponin (119 pg/mL) were among the laboratory tests performed. A computed tomography (CT) scan of the chest was requested ( ), which demonstrated the presence of Hampton’s hump, a pleural-based opacification in the lung most commonly due to pulmonary embolism. Moreover, consolidative pulmonary opacities and peripheral ground-glass areas, both multifocal and bilateral, associated with septal thickening, with a small area of consolidation in between, more accentuated in the right lower lobe and with moderate pulmonary involvement (25-50%) were also found. On 06/25/2020, a computed tomography pulmonary angiogram (CTPA) was also requested ( ), which demonstrated filling defects in the pulmonary arteries bilaterally, extending to its upper, middle and lingual branches, compatible with massive acute pulmonary thromboembolism. The patient was transferred on 06/25/2020 to the Intensive Care Unit (ICU), hemodynamically stable, and then nasal swab and oropharynx material collection for SARS-CoV-2 was requested, which came back with a positive diagnosis on 06/26/2020. Therapy was started with Ceftriaxone (2g daily), Azithromycin (500mg daily), Dexamethasone (6mg daily) and Oseltamivir (75mg daily), associated with Enoxaparin (80mg full dose) as prophylaxis for venous thrombosis. The patient showed progressive improvement. He was discharged from the ICU to the infirmary on 06/28/2020 and on 06/29/2020 he was discharged from the hospital, using Rivaroxaban (15mg BID), being referred for future outpatient reassessment. After the discharge, tests were requested to investigate thrombophilia, including: Functional Protein S, Functional Protein C, Homocysteine, Leiden Factor V, Prothrombin gene mutation, Antithrombin III, Lupus Anticoagulant and Anticardiolipin IgM. The increase in Antithrombin III (999%), the weak presence of Lupus Anticoagulant (1.43) and undetermined IgM Anticardiolipin levels stand out. In addition, echocardiography and Doppler ultrasonography of the lower limbs were requested, which were both within normal standards, ruling out possible signs of thrombosis, either recent or late.
[…]
27,514