Arq. Bras. Cardiol. 2025; 122(5): e20240555
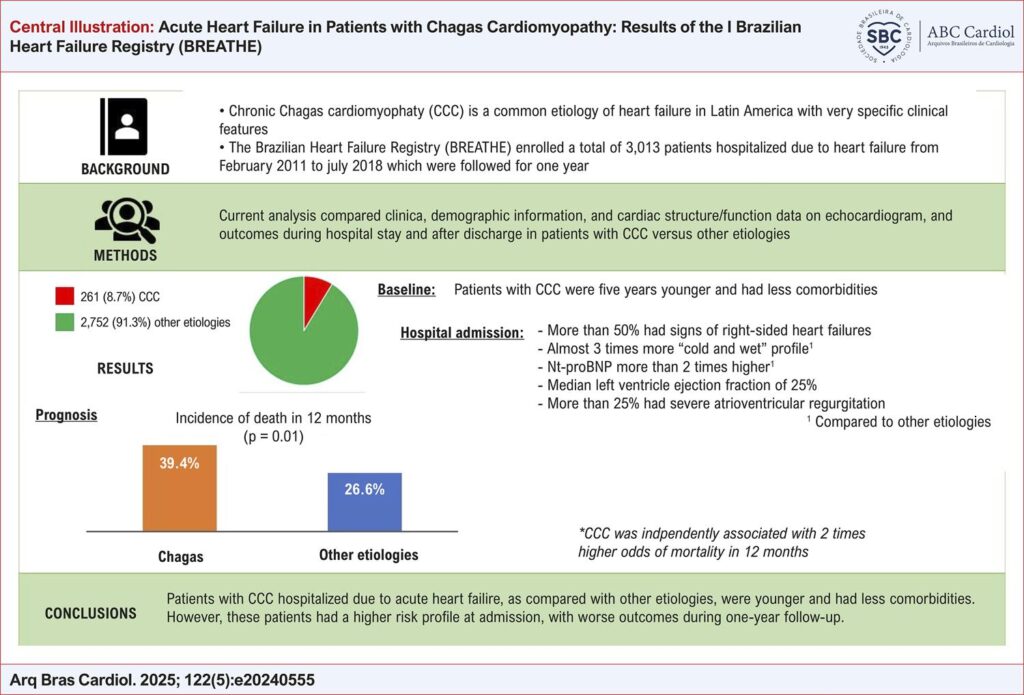
Acute Heart Failure in Patients with Chagas Cardiomyopathy: Results of the I Brazilian Heart Failure Registry (BREATHE)
This Original Article is referred by the Short Editorial "Acute Heart Failure Due to Chagas Disease: Still a Challenge in the 21st Century".
Abstract
Background
Although the clinical features of chronic Chagas’ cardiomyopathy (CCC) have been well established, clinical data about the patients are scarce.
Objectives
The current analysis reports the results of the I Brazilian Heart Failure Registry (BREATHE) assessing baseline characteristics and clinical outcomes of patients with acute heart failure due to CCC.
Methods
BREATHE enrolled a total of 3,013 adult patients hospitalized with acute heart failure. We analyzed comparatively 261 (8.7%) patients with chronic CCC and 2,752 (91.3%) patients with other etiologies. Clinical and demographic information, cardiac structure/function data on echocardiogram and outcomes during the hospital stay and after discharge were assessed in both groups. Uni and multivariate tests were performed and a p-value <0.05 was considered statistically significant.
Results
Patients with CCC presented lower systolic blood pressure (108.3 ± 26.1 vs 128.3 ± 30.3 mmHg, p<0.001) and left ventricle ejection fraction (25.4 [19 - 36]% vs 37 [27 - 54] %, p<0.001) with higher rates of jugular vein distension (54.8% vs 38.9%, p<0.001), hepatomegaly (47.9% vs 25.6%, p<0.001), and “cold and wet” clinical hemodynamic profile (27.2% vs 10.6%, p<0.001). Patients with CCC presented higher rate of the composite death or heart transplantation (17.4% vs. 11.1%, p=0.004), and higher cumulative incidence of death after 3 months (16.5% vs 10.8%, p=0.017), 6 months (25.3% vs 17.2%, p=0.006), and 12 months (39.4% vs 26.6%, p<0.001). Besides, CCC was independently associated with 12-month mortality risk with odds ratio = 2.02 (95% IC: 1.47-2.77).
Conclusion
Patients with CCC, hospitalized due to acute heart failure, in comparison to other etiologies, presented a higher risk profile that was associated with a poorer outcome during hospital stay and after discharge.
585