Arq. Bras. Cardiol. 2023; 120(6): e20220933
An Atypical Non-Cardiac Presentation of Hypertrophic Cardiomyopathy
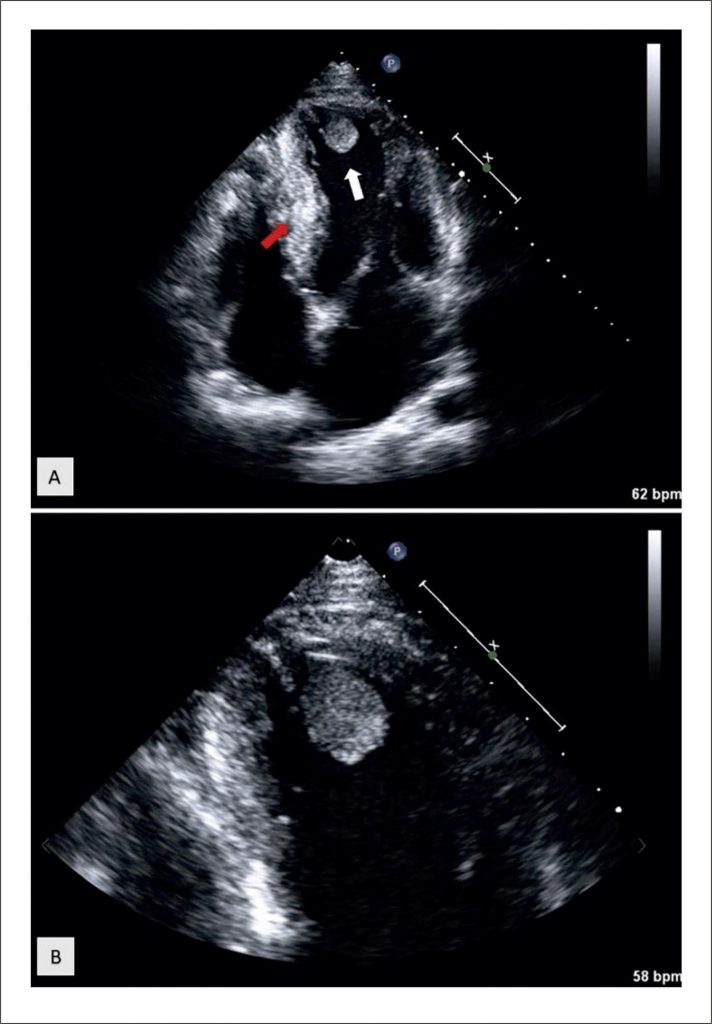
A 33-year-old Brazilian man was admitted to the emergency department with sudden onset of global aphasia and right hemiparesis. An urgent CT angiography of the cerebral arteries confirmed the stroke diagnosis, showing an occlusion of the left internal carotid artery. The patient underwent systemic thrombolysis and mechanical thrombectomy with subsequent neurological improvement. Considering the stroke diagnosis in a young adult most likely of cardioembolic origin, he undertook a thorough diagnostic workup. Of importance, he had a family history of cardiomyopathy, namely his father with hypertrophic cardiomyopathy (HCM) and his grandfather with Chagas disease. However, the patient had no cardiac symptoms (such as exertional dyspnea, chest pain, palpitations, or syncope), cardiovascular risk factors, or history of illicit drug abuse, and he had not performed heart tests since his youth. During hospitalization, his electrocardiogram showed sinus rhythm (68/minute) with T-wave inversion in inferior leads (II, III, aVF), leads I and V6, but no criteria for left ventricular (LV) hypertrophy. He also performed a 24-hour Holter monitoring, ruling out atrial fibrillation or other arrhythmias. Transthoracic echocardiography ( Figure 1 , Supplementary Video 1, Supplementary Video 2) revealed moderate asymmetric septal LV hypertrophy (interventricular septum thickness 14 mm, posterior wall thickness 9 mm), mildly reduced LV ejection fraction (45%), apical akinesia, and an image suggestive of thrombus, explaining the cardioembolic stroke. Cardiovascular magnetic resonance (CMR) confirmed the diagnosis of HCM, with extensive apical fibrosis and akinesia of the apical segments, outlining an apical aneurysm and thrombus ( Figure 2 ). Coronary angiography was performed regarding the possibility of concomitant ischemic heart disease, ruling out obstructive coronary artery disease. Serologic examination for Trypanosoma cruzi was negative. The patient was started on systemic anticoagulation with a vitamin K antagonist (VKA). Considering the diagnosis of HCM with extensive apical fibrosis and an apical aneurism, after patient-shared decision-making, it was decided to place a subcutaneous implantable cardioverter-defibrillator (S-ICD). He was discharged after 18 days. At the 1-year follow-up, control transthoracic echocardiography showed complete resolution of the apical thrombus, and the patient remained on systemic anticoagulation with a VKA.
[…]
1,267