Arq. Bras. Cardiol. 2024; 121(1): e20220784
Clinical and Laboratory Data Up on Hospital Admission are Predictors of New-Onset Atrial Fibrillation in Patients Hospitalized Due to COVID-19 Pneumonia
This Original Article is referred by the Short Editorial "COVID-19 and Atrial Fibrillation: Predicting to Prevent".
Abstract
Background
New-onset atrial fibrillation (NOAF) occurs in patients hospitalized due to COVID-19. It is still unknown whether clinical and laboratory data assessed upon hospital admission have predictive value for NOAF.
Objectives
To analyze, upon hospital admission, variables with predictive potential for the occurrence of NOAF in patients with COVID-19 pneumonia.
Methods
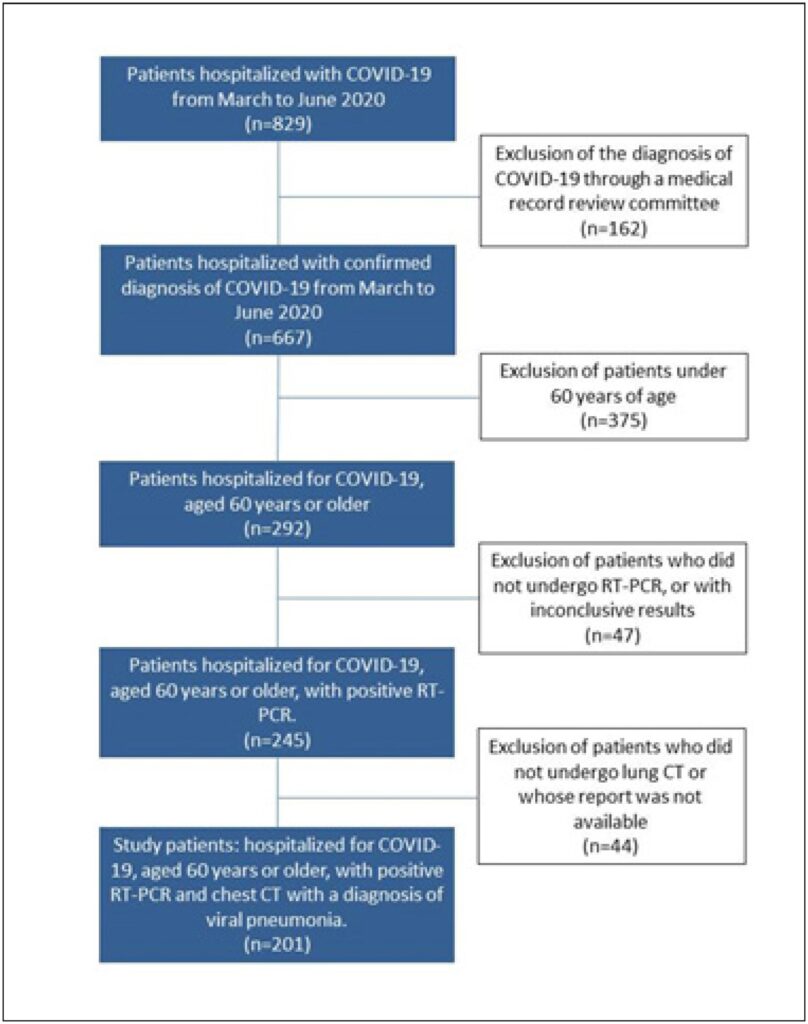
Observational, retrospective, case-control study. Electronic medical reports of consecutive patients, 60 years of age or older, hospitalized due to COVID-19 pneumonia between March 1st and July 15th, 2020, were reviewed. Non-paired Student or chi-squared tests compared variables. A Cox proportional hazard model was employed to identify independent predictors of NOAF. P value < 0.05 was considered statistically significant.
Results
Among 667 patients hospitalized due to COVID-19, 201 (30.1%) fulfilled the inclusion criteria. NOAF was documented in 29 patients (14.4%), composing group 1. Group 2 was composed of 162 patients without NOAF. Ten patients were excluded due to the AF rhythm upon hospital admission. In groups 1 and 2, there were differences in overall in-hospital survival rate (24.1 % vs. 67.9%; p<0.001), length of stay in ICU (11.1 ± 10.5 days vs. 4.9 ± 7.5 days; p=0.004) and need for mechanical ventilation rate (82.9% vs. 32.7%; p<0.001). In the Cox model, age > 71 y/o (HR=6.8; p<0.001), total leukocyte count ≤ 7,720 cels.μL-¹ (HR=6.6; p<0.001), serum [Na+] ≤ 137 mEq.L-¹ (HR=5.0; p=0.001), SAPS3 score > 55 (HR=5.6; p=0.002), and disorientation (HR=2.5; p=0.04) on admission were independent predictors of NOAF.
Conclusion
NOAF is a common arrhythmia in elderly hospitalized patients with COVID-19 pneumonia. Clinical and laboratory parameters evaluated on admission have a predictive value for the occurrence of NOAF during hospitalization.
446