Arq. Bras. Cardiol. 2025; 122(3): e20240447
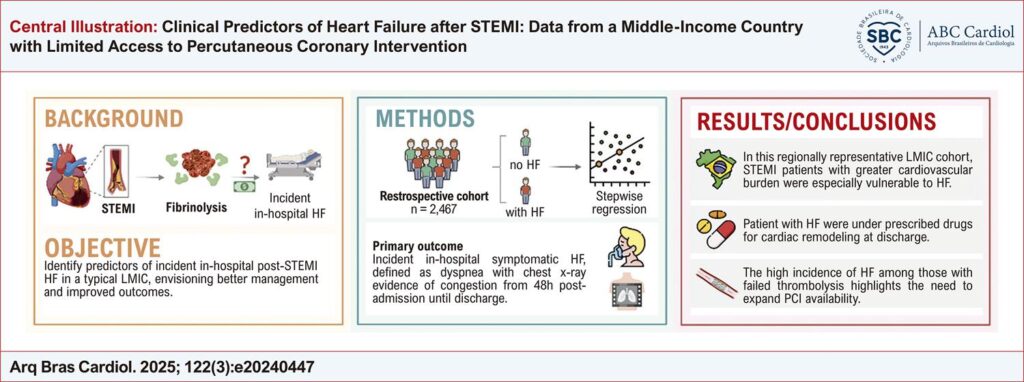
Clinical Predictors of Heart Failure after STEMI: Data from a Middle-Income Country with Limited Access to Percutaneous Coronary Intervention
Abstract
Background
Heart failure (HF) is a common complication of ST-elevation myocardial infarction (STEMI) in low- and middle-income countries (LMICs), where cardiovascular mortality is disproportionately high. Primary percutaneous coronary intervention (PCI) has reduced post-STEMI HF incidence in high-income countries. However, access to this standard of care is poor in LMICs, and data in these settings remain scarce
Objective
To identify predictors of HF following STEMI in a LMIC with limited access to PCI, aiming at better management and outcomes.
Methods
This retrospective cohort study analyzed 2,467 STEMI patients admitted to two Brazilian public hospitals between January/2015 and February/2020. All participants received pharmacological thrombolysis and underwent coronarography within 48h post-admission. The primary outcome was symptomatic HF, defined as dyspnea with chest X-ray evidence of congestion, from 48h post-admission until discharge. Stepwise binary logistic regression was used to identify HF predictors. Significance was defined as p-values<0.05.
Results
The population was 61.9% male, mean age was 58.3±12.6 years, and 39.9% developed post-STEMI HF. HF was more common among older men with cardiovascular-kidney-metabolic (CKM) disease, larger infarcts, and left anterior descending artery involvement. Medications were often underprescribed at discharge, especially aldosterone antagonists (11.0%). HF was notably more frequent among individuals with failed thrombolysis (47.0%).
Conclusions
This regionally representative cohort from a LMIC with limited access to PCI showed that older men with CKM disease are particularly vulnerable to post-STEMI HF, and that HF pharmacotherapy at discharge needs optimization. The high HF incidence among patients with failed thrombolysis highlights the need to expand PCI availability.
528