Arq. Bras. Cardiol. 2025; 122(7): e20250056
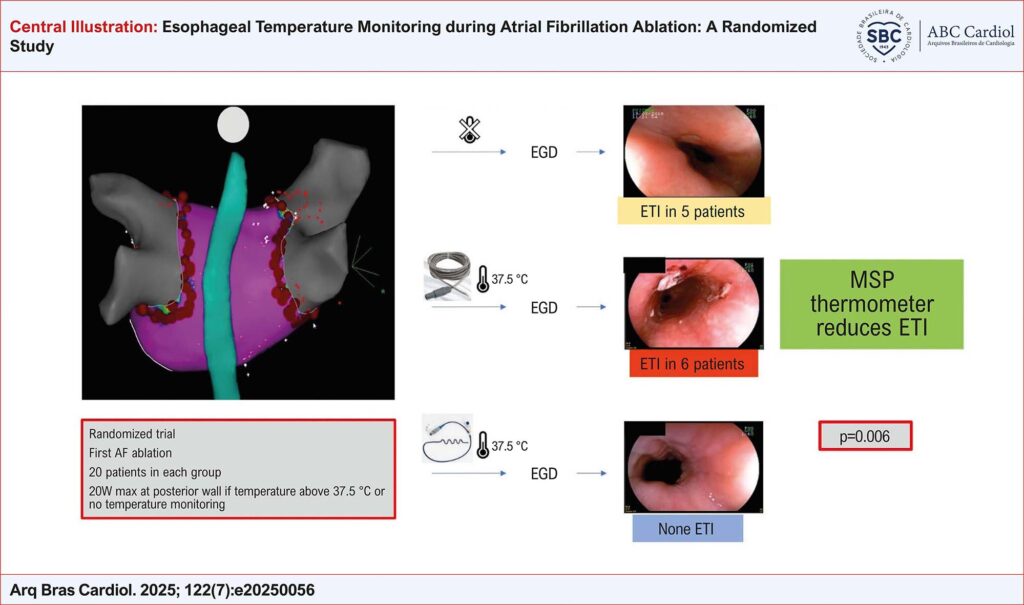
Esophageal Temperature Monitoring during Atrial Fibrillation Ablation: A Randomized Study
Abstract
Background
Pulmonary vein isolation (PVI) for atrial fibrillation (AF) ablation carries a risk of esophageal thermal injury (ETI), which can lead to severe complications.
Objective
To evaluate three luminal esophageal temperature (LET) monitoring strategies and assess their effectiveness in reducing the incidence of ETI.
Methods
Patients with AF were randomized into three PVI groups according to the temperature monitoring strategy: no LET monitoring (Group 1), LET monitoring with a single-sensor probe (SSP) thermometer (Group 2), and LET monitoring with a multisensor probe (MSP) thermometer (Group 3). In Group 1, AF ablation was performed at a fixed power of 20 W on the left atrial posterior wall. In Groups 2 and 3, AF ablation power was titrated based on LET measurements, with a cutoff temperature of 37.5 °C. Each group included 20 patients. A two-sided p-value <0.05 was considered statistically significant. The trial was registered on ClinicalTrials.gov (#NCT03645070) and International Clinical Trials Registry Platform (#RBR-2yvgyf).
Results
All patients underwent PVI and esophagogastroduodenoscopy. No ETI was observed in patients monitored with an MSP thermometer. In contrast, five patients without LET monitoring and six patients monitored with an SSP thermometer developed ETI (p=0.006). Higher temperatures were recorded with an MSP thermometer (37.9 vs. 38.45 °C, p=0.018). There were no significant differences in PVI duration or total radiofrequency application time (p=0.250 and p=0.253, respectively).
Conclusions
LET monitoring with an MSP thermometer during PVI significantly reduces the incidence of ETI compared to no monitoring or SSP monitoring. Implementing advanced LET monitoring strategies may enhance patient safety without compromising procedural efficiency.
161