Arq. Bras. Cardiol. 2021; 116(3): 404-412
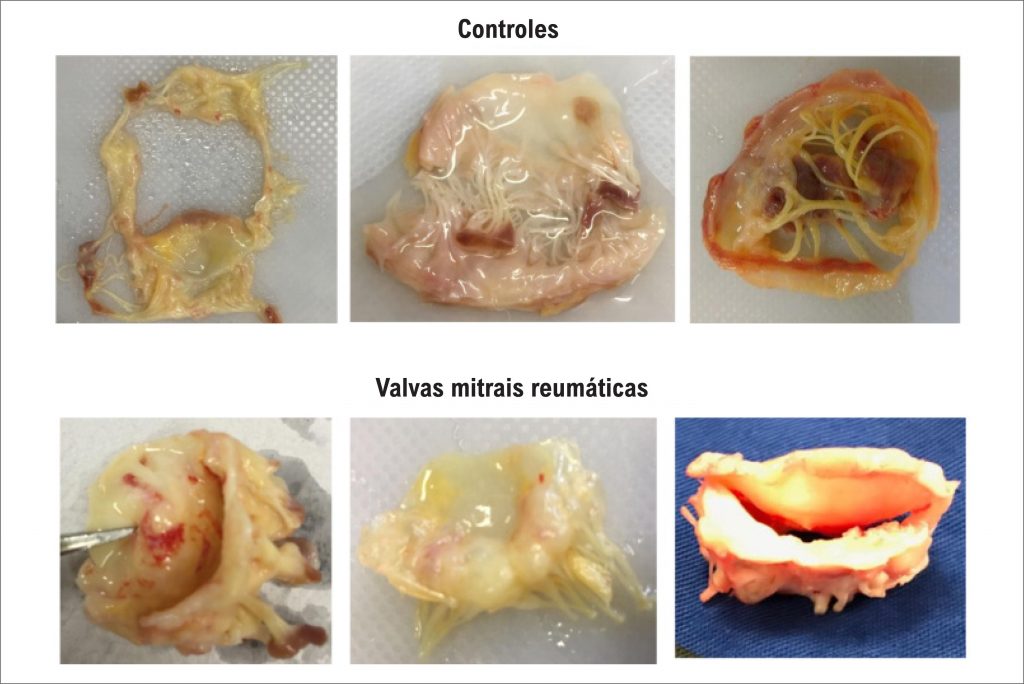
Histopathological Characterization of Mitral Valvular Lesions from Patients with Rheumatic Heart Disease
This Original Article is referred by the Short Editorial "Histopathological Characterization of Mitral Valvular Lesions in Patients With Rheumatic Heart Disease: Is Inflammation Also to Blame for Chronic Valvular Heart Disease Progression?".
Abstract
Background:
The underlying mechanisms by which rheumatic heart disease (RHD) lead to severe valve dysfunction are not completely understood.
Objective:
The present study evaluated the histopathological changes in mitral valves (MV) seeking an association between the pattern of predominant valvular dysfunction and histopathological findings.
Methods:
In 40 patients who underwent MV replacement due to RHD, and in 20 controls that underwent heart transplant, histological aspects of the excised MV were analyzed. Clinical and echocardiographic data were also collected. Histological analyses were performed using hematoxylin-eosin staining. Inflammation, fibrosis, neoangiogenesis, calcification and adipose metaplasia were determined. A p value<0.05 was considered to be statistically significant.
Results:
The mean age of RHD patients was 53±13 years, 36 (90%) were female, whereas the mean age of controls was 50±12 years, similar to the cases, with the majority of males (70%). The rheumatic valve endocardium presented greater thickness than the controls (1.3±0.5 mm versus 0.90±0.4 mm, p=0.003, respectively), and a more intense inflammatory infiltrate in the endocardium (78% versus 36%; p=0.004), with predominance of mononuclear cells. Moderate to marked fibrosis occurred more frequently in rheumatic valves than in control valves (100% vs. 29%; p<0.001). Calcification occurred in 35% of rheumatic valves, especially among stenotic valves, which was associated with the mitral valve area (p=0.003).
Conclusions:
Despite intense degree of fibrosis, the inflammatory process remains active in the rheumatic mitral valve, even at late disease with valve dysfunction. Calcification predominated in stenotic valves and in patients with right ventricular dysfunction.
3,885