Arq. Bras. Cardiol. 2022; 119(1): 128-132
Reinnervation after Renal Denervation – A Myth?
Introduction
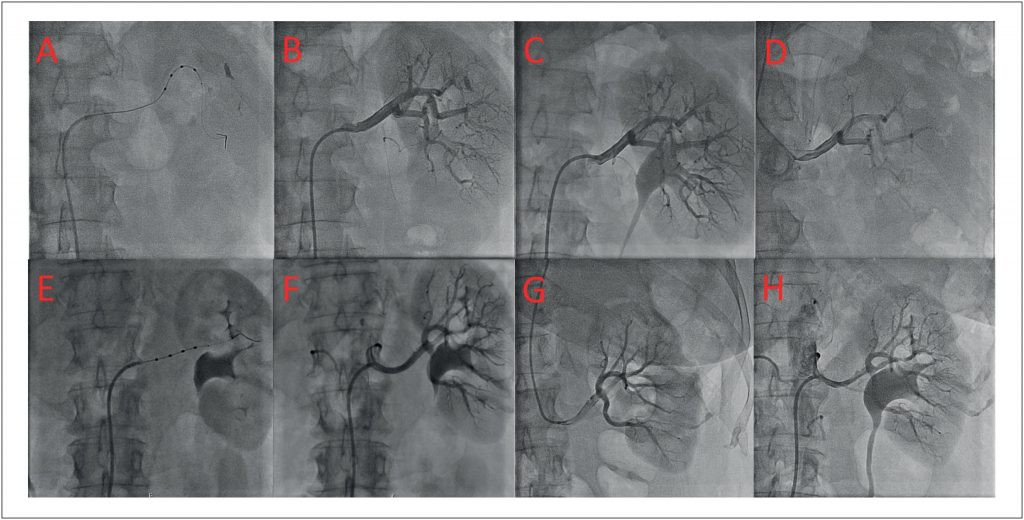
Hypertension (HTN) is a leading risk factor influencing the global burden of cardiovascular disease. In spite of the fact that measures such as lifestyle changes and pharmacological treatment reduce blood pressure (BP) and cardiovascular complications, worldwide, the treatment of HTN remains suboptimal with inadequately controlled BP in many patients. In the ReHOT Randomized Study, the prevalence of resistant HTN was 11.7% among Brazilian hypertensive patients, which is in agreement with the prevalence reported in other international studies., According to the current guidelines of the European Society of HTN, resistant HTN is defined when target BP values are not reached, despite prescription of triple therapy, including a diuretic at a maximum tolerated dose. Sympathetic nervous system hyperactivity is thought to play a major role in resistant HTN. At the kidney level, the efferent sympathetic outflow to the kidneys leads to increased noradrenaline production, renal vasoconstriction and renin release, causing sodium retention. On the other side, afferent sympathetic fibers send signals to the brain to stimulate central sympathetic activity and contribute to neurogenic HTN. Catheter-based renal denervation (RDN) has emerged as one of the most frequently used invasive methods for the treatment of resistant HTN. It aims to ablate the afferent and efferent sympathetic nerves in the adventitia of the renal arteries using radiofrequency energy. It is performed through the insertion of the device catheter percutaneously into the femoral artery, which is then advanced into the main renal arteries under fluoroscopic guidance. According to a meta-analysis, the rate of procedural complications is low and consists mainly in pseudoaneurysms at the vascular access site and renal artery dissection. Nevertheless, its role in clinical practice is controversial and there is scarce information about the different responses to this procedure. We report two cases of idiopathic resistant HTN treated with RDN. Both patients had a profound initial response to the procedure. Nevertheless, their BP was back to baseline values at the 24 and 18-month follow-up, respectively. An investigation to detect secondary causes of HTN was performed with no findings that justified the BP changes. Therefore, a new RDN was performed, with good results, lasting until the present day (6-month follow-up for patient 1 and more than 3-year follow-up for patient 2). This is a report about the heterogeneous response to RDN, the possible role of functional re-innervation and the potential development of supersensitivity to norepinephrine after RDN. These mechanisms could be responsible for increasing the BP back to baseline values after an optimal initial response.
[…]
740