Arq. Bras. Cardiol. 2024; 121(6): e20230829
Wide QRS Tachycardias Management in Emergency Departments: What Really Matters
Introduction
Studies have shown that 80% of wide QRS tachycardias are ventricular tachycardias (VT). This number rises to 90% if there is underlying structural heart disease.– Criteria for differentiating between VT and supraventricular tachycardia (SVT) exist, and they are important in clinical practice, but not necessarily for the purpose of providing an exact diagnosis in acute settings.–
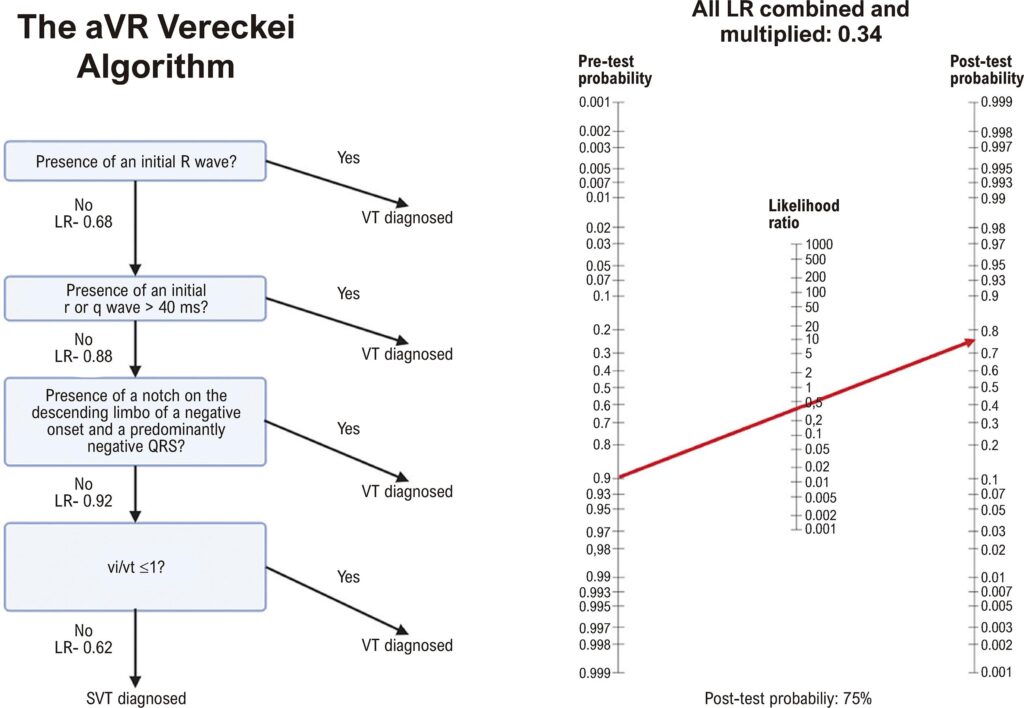
Although the criteria have been validated, they are not as effective at ruling out conditions as one might think. A real-world study showed that Vereckei’s criteria had a negative likelihood ratio of 0.34. This means that applying these criteria to a patient with a 90% pre-test probability would still result in a post-test probability of 75% for VT (). In that study, the Brugada criteria yielded a similar negative likelihood ratio of 0.24, resulting in a 68% probability for VT. Another reason not to rely solely on these criteria is the absence of baseline electrocardiogram (ECG) data. For instance, a patient with congenital heart disease may have a northwest axis and other unique findings. Similarly, a patient with Purkinje fiber blockage and electrically inactive zones may present with misleading ECG features., Adding to the complexity, idiopathic VT, such as fascicular VT, often present ECG patterns that mimic bundle branch or fascicular blocks, leading to misinterpretation. Another emblematic case is bundle-branch reentry VT, where the ECG during tachycardia will display morphological criteria of either left or right bundle branch block, further confounding the diagnosis.
[…]
3,308