Arq. Bras. Cardiol. 2022; 119(4): 531-532
Conduction Disturbances Associated with Transcatheter Aortic Valve Implantation: Challenge for another 20 Years?
This Short Editorial is referred by the Research article "Long-Term Ventricular Pacing Dependency and Pacemaker Implantation Predictors after Transcatheter Aortic Valve Replacement – A 1-Year Follow-Up".
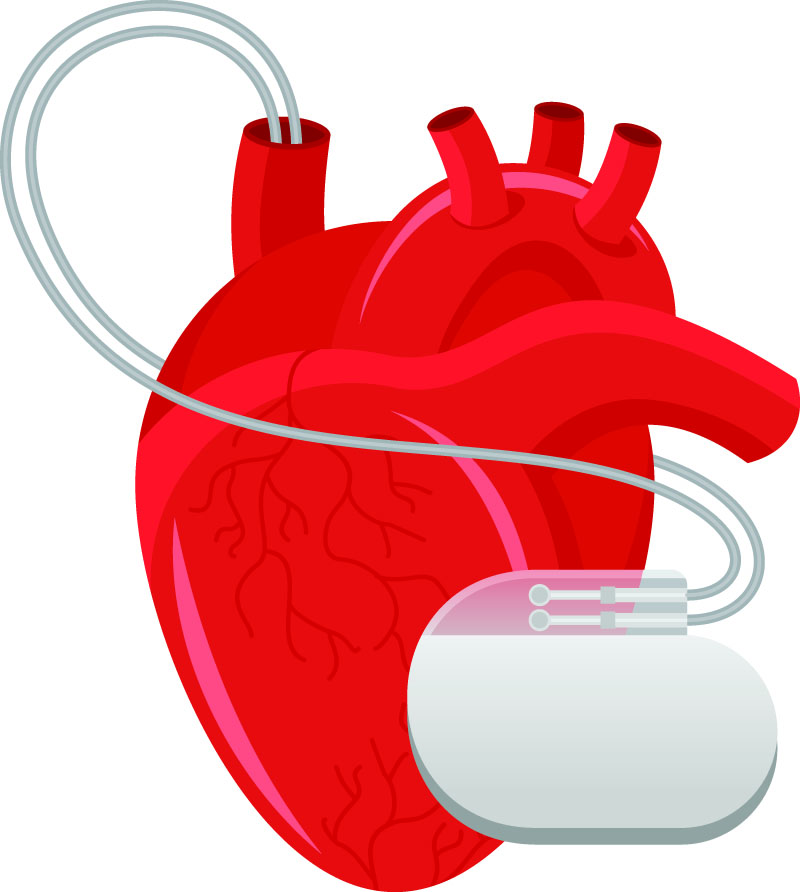
Transcatheter aortic valve implantation (TAVI) is a well-established procedure for treating severe aortic stenosis in elderly patients, regardless of the surgical risk. Since its introduction two decades ago, there have been major technological advances in devices, which, combined with new implantation techniques, have brought significant reductions in periprocedural complication rates, leading to their greater adoption worldwide. However, the incidence of conduction disorders showed a modest reduction, remaining the most frequent complication after TAVI, – which contributes to the increase in hospital stay, costs and the worsening of short and long-term clinical outcomes. In addition, the approach to conduction disorders still varies greatly between centers, especially regarding the management of new left bundle branch block (LBBB), post-procedure advanced atrioventricular block (AVB) and previous right bundle branch block (RBBB), translated into variable rates of permanent pacemaker (PM) implantation. Among patients who received PM after TAVI, there is also great variability regarding their dependence (ventricular pacing) at follow-up.
In this journal edition, Pinto et al. evaluated the incidence of conduction disorders, predictors and the rate of PM dependence in a population of 340 consecutive patients undergoing TAVI. Conduction disorders occurred in more than 50% of post-procedure patients, with LBBB being the most frequent (32%), showing spontaneous resolution in 56% of them after 6 months. The overall PM implant rate was 18.5%, with prior RBBB being its main predictor. Among the patients who required PM, the main reasons were advanced AVB (60.3%), followed by LBBB with low-degree AVB (22%). Interestingly, there was a wide variation in the percentage of ventricular pacing among patients who received PM, being 83% in patients with advanced AVB (Advanced AVB and Mobitz Type II) and only 2% in those implanted with LBBB and low-degree AVB (first-degree AVB and Mobitz type I). – However, some aspects of this study deserve reflection.
[…]
Keywords: Conduction Disturbances; Pacemaker; TAVI
677