Arq. Bras. Cardiol. 2024; 121(11): e20240701
Worse Prognosis of STEMI Patients during Off-Hours: What are we Missing?
This Short Editorial is referred by the Research article "Primary Percutaneous Coronary Intervention during Off-Hours: One-Decade Experience from a High-Volume Cardiovascular Center".
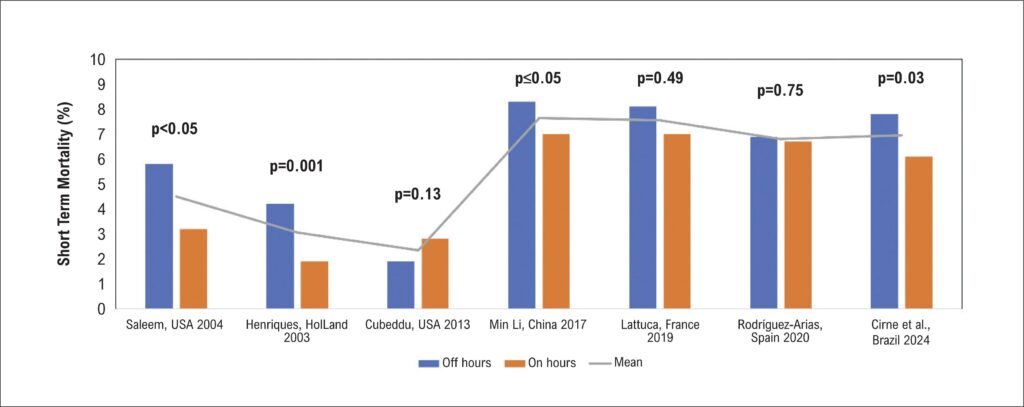
In Brazil, the annual incidence of myocardial infarction is estimated at approximately 300,000 to 400,000 cases. Despite advancements in treatment, myocardial infarction remains the leading cause of death in Brazil and globally, with a lethality rate of around 9%. According to the BRACE registry, acute coronary syndrome (ACS) accounts for 45% of hospitalizations in Brazil, with two-thirds attributed to acute myocardial infarction (AMI), including both ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI). Notably, 40% to 60% of STEMI patients present during off-hours, between 7 PM and 7 AM, and on weekends., Given that the treatment of STEMI is time-sensitive and requires a complex multidisciplinary team in the catheterization laboratory, the impact of presentation timing on patient outcomes remains a contentious issue. Thus, the question of whether off-hours presentation results in a poorer prognosis is still debated.
In this issue of the journal, Cirne et al. examined a prospective registry from a high-volume ACS center in Southern Brazil, encompassing 4,436 consecutive STEMI patients who underwent primary percutaneous coronary intervention (PPCI) between 2009 and 2019. Patients were stratified by presentation time: on-hours versus off-hours. The primary outcome was a composite of major adverse cardiac events (MACE), which included death, AMI, or stroke at one year, along with MACE at 30 days, stent thrombosis, and the need for new revascularization. Among the cohort, 2,576 (57%) patients were treated during off-hours, with no significant differences between the groups concerning age, sex, infarction-related artery, or Killip classification. Additionally, symptom-to-hospital time (mean 240 minutes) and door-to-balloon time (DTB) (mean 70 minutes) were similar. No differences were observed in procedural complexity, complications, intra-aortic balloon pump usage, or angioplasty success rates; however, off-hours patients exhibited a higher thrombotic burden (49.6% vs. 45.5%, p<0.01). Despite comparable baseline clinical and angiographic characteristics, those presenting off-hours had higher rates of MACE at 30 days and one year (10.2% vs. 8.5% and 15.4% vs. 13.1%, respectively), as well as increased mortality (in-hospital: 7.9% vs. 6.1%; 30 days: 7.8% vs. 6.1%; 1 year: 11.1% vs. 9%, respectively). No differences were noted in AMI or stroke incidence.
[…]
Keywords: Acute Coronary Syndrome; Off-hours; STEMI
161